The approach is based on curriculum called See Think Act, which was created by a U.K.-based expert named Elizabeth Allen and published by the Royal College of Psychiatrists. Hospital leaders invited Ms. Allen to come and train staff in July 2018, when the Forensic Psychiatric Hospital became the first facility in Canada to adopt the approach. The results so far are encouraging—aggressive incidents have dropped significantly.
Allen returned to BC Mental Health and Substance Use Services in June 2018 for another round of training, bringing the number of trained staff at the hospital to over 300. At the end of the training period, Allen and some of our experts shared their experience with therapeutic and relational security on a panel.
In this interview, Allen tells us about the origins of therapeutic and relational security (known in the U.K. as relational security) and how she came to be an international pioneer.
"In mental health services in the U.K., we've been accustomed to considering security at three levels: physical, procedural and relational," Allen says. "But in practice, what we found is that relational security wasn't well enough defined for our staff, so many people made reference to the idea of relational security, but struggled to properly describe it. And for that reason, it was difficult for them to understand when they were delivering relational security, and when they weren't."
The key to relational security is recognizing is that the relationships between staff and patients are vital to developing a safe environment, she explains. Staff who have a thorough understanding of patients, their past traumas, triggers and how they relate to others will often be able to stop harmful incidents before they happen.
"We had a wave of serious incidents in secure facilities the U.K. in about 2009, which, understandably, drew the attention of our government leaders," she says. "They wanted to know how we could prevent such serious incidents from happening and what more physical security was needed in the hospitals where those services were provided. I told them that while services didn't yet have perfect physical security, that wasn't where we needed to focus our attention.
"Leaders were persuaded that rather than more physical security, what was needed was an improvement in relational security. I started with a review of incidents across the full spectrum of mental health services, mapping the learning from all of them into one framework. I think this was the first time we'd done such a comprehensive compilation of learning in mental health."
Through reviewing incidents in secure mental health facilities in the U.K., Allen observed that there were often subtle precursor signs in patient behaviour in the lead-up to an incident. Staff particularly attuned to these indicators might be better able to prevent harm to a patient, physician or staff member before the incident ever unfolded.
"We provided a more meaningful definition of relational security for staff, and explained what we meant and what services might look like if they were getting it right," Allen continues.
"As a result of this work, I set out the model for relational security in See Think Act, the guide to relational security for people working in high-, medium- and low-security mental health services. Despite it being aimed at secure mental health services, though, it's frequently used in other services. I think the principles are the same across the full spectrum of mental health care."
Therapeutic and relational security relies on every member staff at every level in the organization taking responsibility for the care they provide and for saying something if they spot something wrong.
"If you try to understand a patient by relying only on the psychiatrist's assessment, you get a very small picture of the patient and of the service. Our health care workers, for example, have far more day-to-day interactions with patients, so they can provide a significant proportion of the information we need to provide safe care," Allen says.
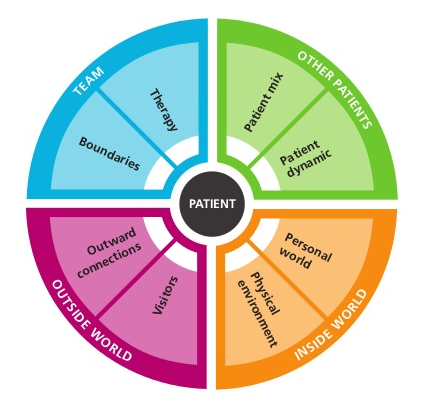
This wheel graphic forms the basis of the See Think Act guide.
"With relational security, there is greater focus on care planning and outcomes. Staff develop care plans so patients understand what's required of them to move on and can be involved in their own care. When this is properly enacted, we see a decrease in violent incidents, an increase in patient participation in treatment, and an increase in meaningful engagement and therapeutic trust between staff and patients," Allen says.
"Relational security and good care planning rely on challenging conventional clinical hierarchies in these settings. When you bring everyone to the table and give them a voice, you see the value that every member of the team, from kitchen staff to the psychiatrist, brings to reducing risk and to helping the people we care for reach their health goals."
Allen is optimistic about the future of therapeutic and relational security in B.C. "You might say, 'We'll need to change our culture to make this work.' You could also say, 'This work might be the way we could change our culture.'"
As part of last month's training at the Forensic Psychiatric Hospital, Allen worked closely with five nurses in the newly created role of clinical security liaison. They were recently hired in the roles to help develop relational security locally and carry the torch forward.
They will mentor other staff, provide relational security supervision where it's needed, and provide an important resource for the ward to help maintain safety for patients and staff. They will also help educate the wider network of PHSA staff about therapeutic and relational security, bringing it throughout the province of B.C.—and even beyond.
